Press Release: Launch of the HEPRR Programme for East and Southern Africa Date: May 11,…
Multi-country research on antimicrobial resistance in Africa reveals only five of 15 antibiotic-resistant pathogens designated by the WHO as priority pathogens are consistently tested
Study across 14 countries reveals lack of laboratory capacity and erratic use of available antibiotics, finds only 1.3% of medical laboratories conduct any bacteriology testing.
September 15, 2022 (Addis Ababa) – New data released on antimicrobial resistance (AMR) from 14 sub-Saharan countries finds that only five out of the 15 antibiotic-resistant pathogens designated by the World Health Organization (WHO) as priority pathogens are being consistently tested and that all five demonstrated high resistance.
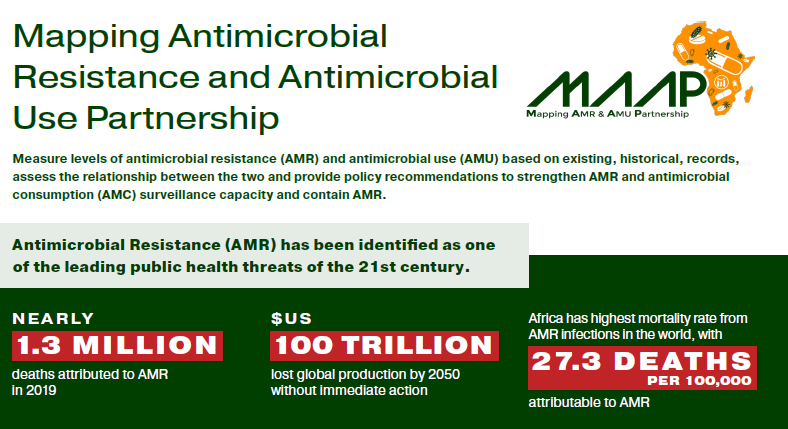
The multi-year, multi-country study was carried out by the Mapping Antimicrobial Resistance and Antimicrobial Use Partnership (MAAP), a consortium spearheaded by the African Society for Laboratory Medicine (ASLM), with partners including the Africa Center for Disease Control and Prevention (Africa CDC), the One Health Trust, the West African Health Organization (WAHO), the East, Central and Southern Africa Health Community (ECSA-HC), Innovative Support to Emergencies, Diseases and Disasters and IQVIA. It provides stark insights on the under-reported depth of the AMR crisis across Africa and lays out urgent policy recommendations to address the emergency.
The results of the study, which was supported by the Fleming Fund, were released on the 15th September 2022 at a meeting held at the African Union. The results provided insight into the AMR burden and antimicrobial consumption in the 14 countries — areas where most available data on AMR is only based on statistical modeling. The efforts by MAAP are the first of their kind to systematically collect, process and evaluate large quantities of antimicrobial resistance and antimicrobial consumption (AMC) data in Africa.
The WHO has repeatedly stated that AMR is a global health priority — and is in fact one of the leading public health threats of the 21st century. A recent study estimated that, in 2019, nearly 1.3 million deaths globally were attributed to antimicrobial resistant bacterial infections. Africa was found to have the highest mortality rate from AMR infections in the world, with 24 deaths per 100,000 attributable to AMR.
MAAP reviewed 819,584 AMR records spanning from 2016 to 2019, from 205 laboratories across Burkina Faso, Ghana, Nigeria, Senegal, Sierra Leone, Kenya, Tanzania, Uganda, Malawi, Eswatini, Zambia, Zimbabwe, Gabon and Cameroon. MAAP also reviewed data from 327 hospital and community pharmacies and 16 national-level AMC datasets.
Researchers found that most laboratories across Africa are not ready for AMR testing. Only 1.3% of the 50,000 medical laboratories forming the laboratory networks of the 14 participating countries conduct bacteriology testing. And of those, only a fraction can handle the scientific processes needed to evaluate AMR. Researchers also found that in eight of the 14 countries, more than half of the population is out of reach of any bacteriology laboratory.
Across the 14 countries clinical and treatment data are not being linked to laboratory results, making it hard to understand what’s driving AMR. Out of almost 187,000 samples tested for antimicrobial resistance, around 88% had no information on patients’ clinical profile, including diagnosis/origin of infection, presence of indwelling device (such as urinary catheters, feeding tubes and wound drains) often associated with development of healthcare-associated infection), comorbidities or antimicrobial usage. The remaining 12% had incomplete information.
The research also found that only four drugs comprised more than two-thirds (67%) of all the antibiotics used in healthcare settings. Stronger medicines to treat more resistant infections (such as severe pneumonia, sepsis and complicated intra-abdominal infections) were not available, suggesting limited access to some groups of antibiotics.
Based on the findings, MAAP is calling for a drastic increase in the quality and quantity of AMR and AMC data being collected across the continent, along with revised AMR National Action Plans.
About AMR
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to antimicrobials, which include antibiotics, antivirals, antifungals and antiparasitics. This makes infections harder to treat and increases the risk of disease spread, severe illness and death.
Given the urgency of the threat of the rise of resistant organisms, the World Health Assembly at its 68th assembly in May 2015, adopted the Global Action Plan on antimicrobial resistance, urged all member states to develop their National Action Plans by 2017 and established the Global Antimicrobial Resistance Surveillance System through which countries are enrolled and encouraged to submit annual AMR surveillance data. In February 2020, African Union (AU) Heads of State and Government committed to addressing the threat of AMR across multiple sectors, especially human health, animal health and agriculture.
Attachments

Related News
Date: June 3-7, 2024 Location: Durban International Conference Centre, Durban, South Africa Join us at…
We're looking for a Software Developer to join the Thanzi La Mawa Research Project in…
